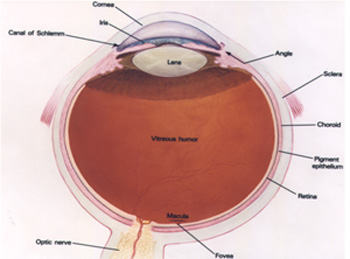
The cornea is the front window to the eye. It allows light into the eye and bends (refracts) the light rays to help the lens focus them upon the retina. To perform properly, the cornea must be crystal clear and be a proper curvature.
What Causes the Cornea to Become Cloudy?
There are many causes for the clouding for the cornea.
They include the following:
Eye injuries that leave a dense white scar on the cornea. These injuries may include
penetrating wounds from a sharp object, burns, or chemical contamination of the eye.
A severe corneal infection that leads to corneal scarring. The infection may be bacterial,
viral, or fungal in origin. Various herpes viruses are known to cause such scarring.
Abnormal shapes of the cornea, caused by diseases such as keratoconus, may scar the center
of the cornea or distort vision so severely that glasses or contact lenses are of little
help.
Corneal dystrophies may cause clouding.
Inherited diseases of the cornea
Cataract or other eye surgery can prompt corneal clouding.
Where Does Corneal Transplant Tissue Come From?
During corneal transplant surgery, only the clear, central part of the cornea is replaced. Corneal tissue used for transplant surgery comes from donors. An eye bank procures the tissue, examines it, and then stores and protects it until used. All tissue used for transplantation is extensively tested. It is screened for the presence of communicable diseases such as hepatitis and the presence of HIV (the AIDS virus).
How is a Corneal Transplant Performed?
The corneal transplant operation may be performed under either a local or general
anesthetic,
depending on what the doctor believes to be in the patient's best interests. The surgeon
removes
the center of the cloudy cornea and replaces it with the clear donor cornea. The donor
tissue is
sewed in place.
If a cataract is present the surgeon can remove it as part of the corneal transplant
operation.
If an artificial lens is already in place in the eye and it is believed to be responsible
for
the clouding of the cornea, the artificial lens can be replaced with a type of lens less
likely
to irritate the donor corneal tissue.
What Happens After A Corneal Transplant Operation?
The eye is patched overnight and examined the next day. Usually, there is little or no
discomfort after surgery. In most cases, resumption of normal activities may occur soon
after surgery with some reasonable limitations. For example, lifting heavy objects or
strenuous exercise must be avoided until directed otherwise by the physician.
Until the eye has healed, glasses or an eye shield must be worn to protect the eye. For
several weeks following the transplant surgery, eye drops will be prescribed. The eye drops
are to prevent infection and rejection of the donor corneal tissue.
The sutures used to sew the donor cornea in place are barely visible and do not cause pain.
It is normal for the eye to feel scratchy or irritated for the first few days following
surgery. As the cornea heals, some of the stitches used to sew the donor tissue into place
are removed. This can be done quite easily in the doctor's office. During the first few
weeks after surgery, vision is usually quite blurry. It takes time for the eye to completely
heal after surgery. It may take four to six months or even longer for the cornea to
stabilize. Once the cornea stabilizes, improved vision is usually enjoyed. Glasses or
contact lenses may be required. In some cases, Astigmatism may be noticeable. Often, this
can be corrected with glasses or contact lenses.
What Are The Risks Of Corneal Transplant Surgery?
Just as is true with any operation, corneal transplant surgery entails some degree of risk. The
success of the transplantation surgery is often related to the original cause of the underlying
corneal disease process.
Transplant procedures resulting from abnormally shaped corneas due to keratoconus or for corneal
clouding following cataract surgery typically have very high success rates. Conversely,
transplants due to scarring of the cornea from infections, such as herpes, typically have a
lower success rate.
Rejection of the transplanted tissue can occur following corneal transplant surgery. Corneal
graft rejection rarely occurs within 2 weeks and may occur as late as 20 years following corneal
transplant. Pain, light sensitivity, redness, and decreasing vision are warning signs of corneal
tissue rejection and indicate the need for immediate medical attention. When started at the
first signs of tissue rejection, steroids (drops, injections, and/or pills) may be effective in
halting the rejection process.
If the rejection process continues, the donor tissue becomes cloudy, resulting in blurry vision.
Often, a repeat transplant may be performed.
The risk always exists that vision could be permanently impaired or lost. Other possible
complications include bleeding, infection, scarring, glaucoma, retinal swelling, retinal
detachment, cataract formation, and swelling of the donor graft.
Although risks are present, the success rate of corneal transplantation is very high. It enjoys
the highest success rate of any transplant procedures commonly performed.